When Supporting Others Costs You Everything: Rebuilding Your Capacity to Care
You became a caregiver to heal others. But you can’t pour from an empty cup. Here’s how to refill yours and keep serving with excellence.
Your alarm goes off at 5:15 AM.
Again.
Your body knows before your mind does.
Your chest tightens.
The familiar dread settles in your stomach like a stone.
You are a counselor. You help people process their trauma, untangle their pain, and rebuild their lives.
But you can’t remember the last time you slept through the night.
Forty-seven clients this month, and most of them are carrying things heavier than you can name.
Domestic violence. Grief. Sexual assault. Poverty. Addiction and complex trauma.
And today, client #48 at 9 AM.
You sit on the edge of the bed, frozen.
What if I have nothing left to give?
Here’s what nobody told you when you started:
You can’t serve from an empty vessel. And somewhere along the way, between the impossible caseloads and the weight of others’ pain, you stopped refilling yours.
The research confirms what you are feeling: 95.4% of medical workers at Kenyatta National Hospital show signs of burnout. In Homa Bay County, 88.7% of nurses report high levels of emotional exhaustion. Among therapists in Eldoret, 70% experience compassion fatigue.
But here’s the truth they don’t tell you: Burnout isn’t permanent. And it doesn’t mean you’re in the wrong profession.
It means you need to learn how to sustain the gift you have.
Before we talk about solutions, let’s make sure you understand what’s really happening. Because recognizing burnout is the first step to healing it.
You’re Not Imagining It: What the Data Shows About Caregiver Burnout in Kenya
First, let’s name what’s happening.
If you’re a nurse, therapist, social worker, counselor, or NGO worker in Kenya feeling depleted, you’re not weak. You’re experiencing something measurable, documented, and most importantly, addressable.
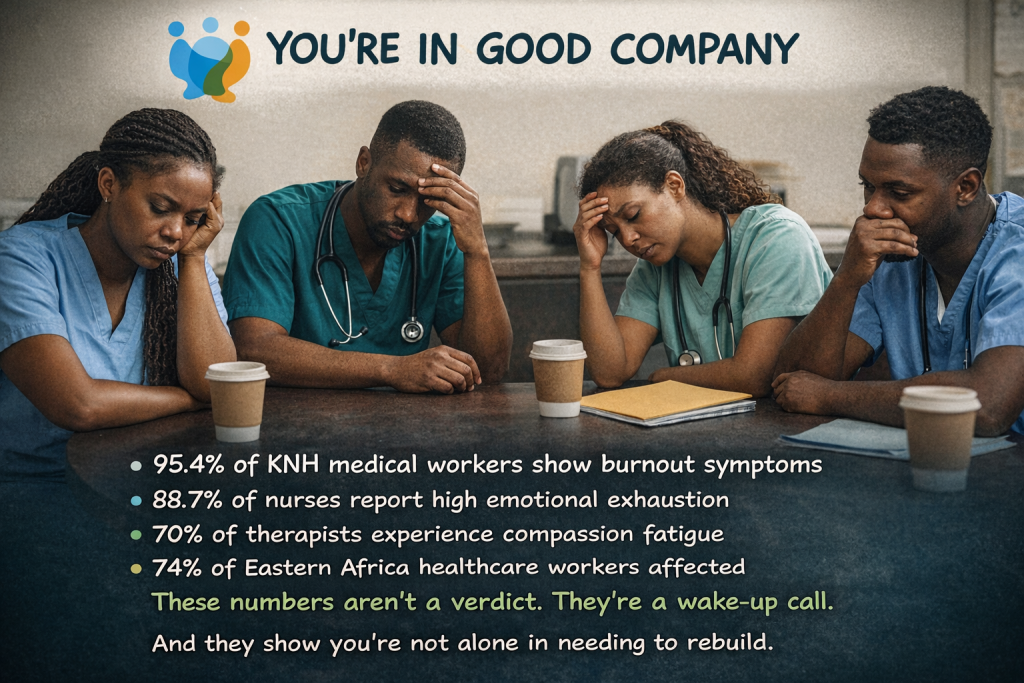
During COVID-19, 47.9% of nurses at Aga Khan University Hospital, Nairobi, were burnt out. Female nurses hit 53.9%. Depression affected 45.9%, anxiety 48.2%, and insomnia 37%.
Only 1.8% had sought help before the crisis hit.
This PLoS One article, published July 1, 2021, surveyed 171 nurses (67.1% response rate) from August to November 2020 using validated tools like PHQ-9 (depression), GAD-7 (anxiety), ISI (insomnia), IES-R (distress), and SPFI (burnout). It reports burnout in 47.9% overall (SPFI score >1.33), with females at 53.9% versus males at 34.0% (p=0.027). Depression affected 45.9%, anxiety 48.2%, and insomnia 37.0% (any severity).
Key Data Table
Condition Overall (%) Females (%) Source Notes Burnout 47.9 53.9 SPFI >1.33; Table 2 Depression 45.9 – PHQ-9 ≥5; Abstract Anxiety 48.2 – GAD-7 ≥5; Abstract Insomnia 37.0 – ISI ≥8; Abstract
They’d been ignoring the warning signs. Pushing through. Believing the lie that asking for help meant professional failure.
This isn’t normal fatigue. This is your body and soul signaling: something needs to change.
But why? Why are so many of us hitting this wall? Understanding the path that led you here is essential to finding your way out.
Why Caregivers Burn Out: Understanding the Path That Led You Here
Burnout doesn’t happen because you’re doing it wrong.
It happens when the demands on you consistently exceed your capacity to meet them, and you haven’t been taught how to protect that capacity.
Let’s be honest about the challenges:
The Workload Reality
Kenya has approximately 1 doctor per 16,000 people. In public hospitals, nurses serve 30–40 patients per shift. There are roughly 100 psychiatrists for 55 million people.
Key Sources Table
Statistic Figure Source (Year) Doctors ratio ~1:16,000 (claimed) Africa Check (2018) Nurses per shift (public) 30–40 patients Standard (2025) Psychiatrists ~150 for 50M+ KPA/Standard (2025)
These aren’t excuses. They’re facts.
And while you can’t fix the healthcare infrastructure alone, you can learn to work within it without destroying yourself.
The Compensation Reality
Entry-level nurses earn ~Ksh 23,369/month. Counselors: Ksh 30,000–60,000. Social workers: Ksh 42,200.
Key Sources Table
Role Salary (Ksh/month) Notes/Source (Year) Entry Nurse 23,369 basic KNUN CBA Job G (2014) Counselors 30,000–60,000 Avg. estimates (2025) Social Workers ~42,200 Public sector entry equiv.
You chose this work knowing it wouldn’t make you rich.
But you didn’t sign up to be financially struggling while emotionally depleted.
The question isn’t whether the pay is fair. The question is: How do you thrive anyway?
The Cultural Expectation
In Kenya, caregiving carries deep cultural weight. It’s a family duty. Community obligation. Especially for women, who make up 75% of nurses and bear the dual burden of professional care and 4–5 hours of daily home care.
Mental health challenges are often seen as spiritual failure. For caregivers, admitting struggle feels like admitting incompetence.
But here’s the correction: Seeking support isn’t a weakness. It’s wisdom.
Even healers need healing. Even guides need guidance.
The Training Gap Nobody Mentions
Most caregiving training programs teach you how to help others. Almost none teach you how to sustain yourself while doing it.
Clinical supervision is rare. Peer support structures are informal at best. Wellness programs are almost nonexistent. Formal employee wellness programs are not standard in Kenyan healthcare.
Kenya’s National Guidelines on Workplace Mental Wellness were only launched in September 2023 by the Ministry of Health, extremely recent, and implementation remains nascent. A Public Service Counselling and Wellness Policy exists at the government level, but is weakly operationalized.
Evidence from Botswana shows that healthcare workers participating in 7+ wellness activities had significantly higher job satisfaction and lower stress and exhaustion, but such programs barely exist in Kenya.
This isn’t about blame. It’s about recognizing: you were sent into deep waters without being taught to swim.
But you can learn now.
Now that you understand the forces creating this crisis, let’s talk about how it shows up in your daily life. Because burnout sends signals before it becomes a catastrophe.
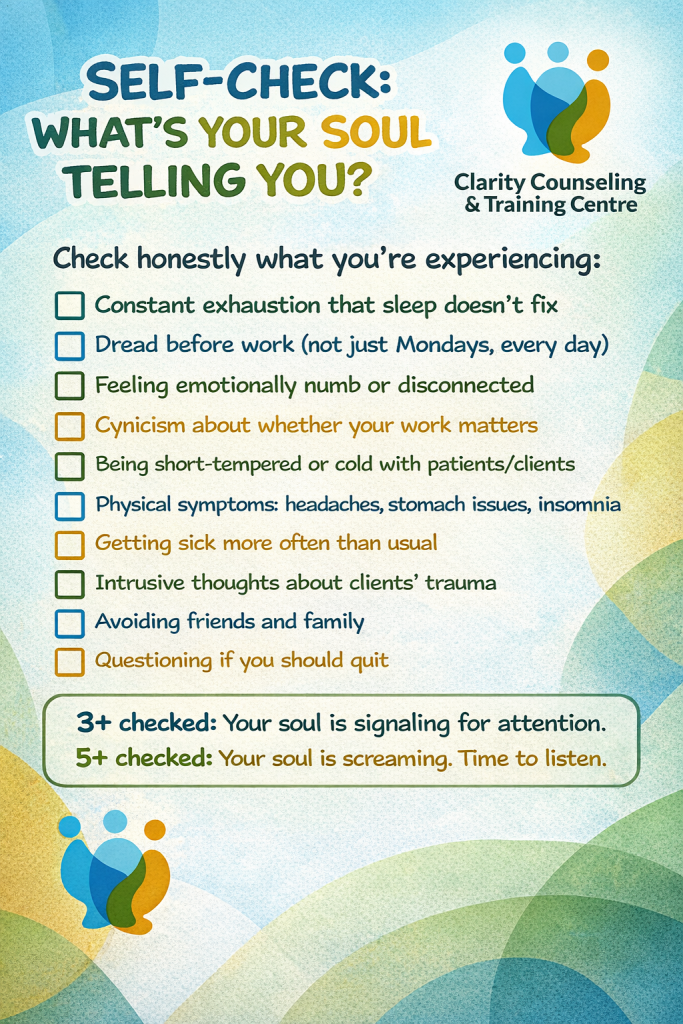
The Warning Signs: Is Your Soul Sending You an SOS?
Your body and spirit have a warning system.
Burnout doesn’t arrive overnight. It sends signals. The question is: Are you listening?
- The alarm goes off. Your chest tightens before you’re even fully awake.
- You sit across from your client. They’re talking. You’re nodding. But you’re not really there.
- You’ve heard this story a hundred times. You used to care deeply. You still do care.
But today? You feel… nothing.
I thought I was supposed to have it all together. But I realized: even healers need healing. Even guides need guidance, Grace, Counselor in Nairobi
So you’ve recognized the symptoms. Now comes the harder question: What happens if you ignore them? Or better, what happens if you don’t?
Two Paths Forward: Which Will You Choose?
You’re standing at a crossroads.
One path is familiar. Keep pushing. Keep ignoring the signals. Keep believing you can white-knuckle your way through.
The other path requires something harder: admitting you need help and doing something about it.
Path 1: Keep Going As You Are and Your:
- Relationships will suffer.
- Health will deteriorate.
- Patients will receive care from someone who’s disconnected.
- Effectiveness will decline.
Eventually, you’ll quit. Not because you wanted to, but because your body forced you to.
Kenya already loses 4,000 healthcare workers annually to burnout and immigration. The patients who need you most lose access to care.
Path 2: Choose Restoration. You:
- Learn you’re not broken, you’re depleted.
- Build boundaries that protect your capacity to care.
- Process the trauma you’ve been absorbing.
- Discover sustainable rhythms of work and rest.
- Stay in the profession. And you’re actually present.
- Clients get the version of you they deserve.
- Get the life you deserve.
Kenya keeps a caregiver it desperately needs.
Which path are you on right now?
If you’re choosing Path 2, restoration, here’s what you need to know. These aren’t vague wellness tips. This is the training you never got.
How to Rebuild Your Capacity to Care: The Training You Never Got
Here’s what most caregiving programs don’t teach you:
Sustainable caregiving requires intentional practices, skills you can learn.
The World Health Organization’s research is clear: individual resilience alone isn’t enough if your environment is toxic. But you can build both personal capacity AND advocate for systemic change.
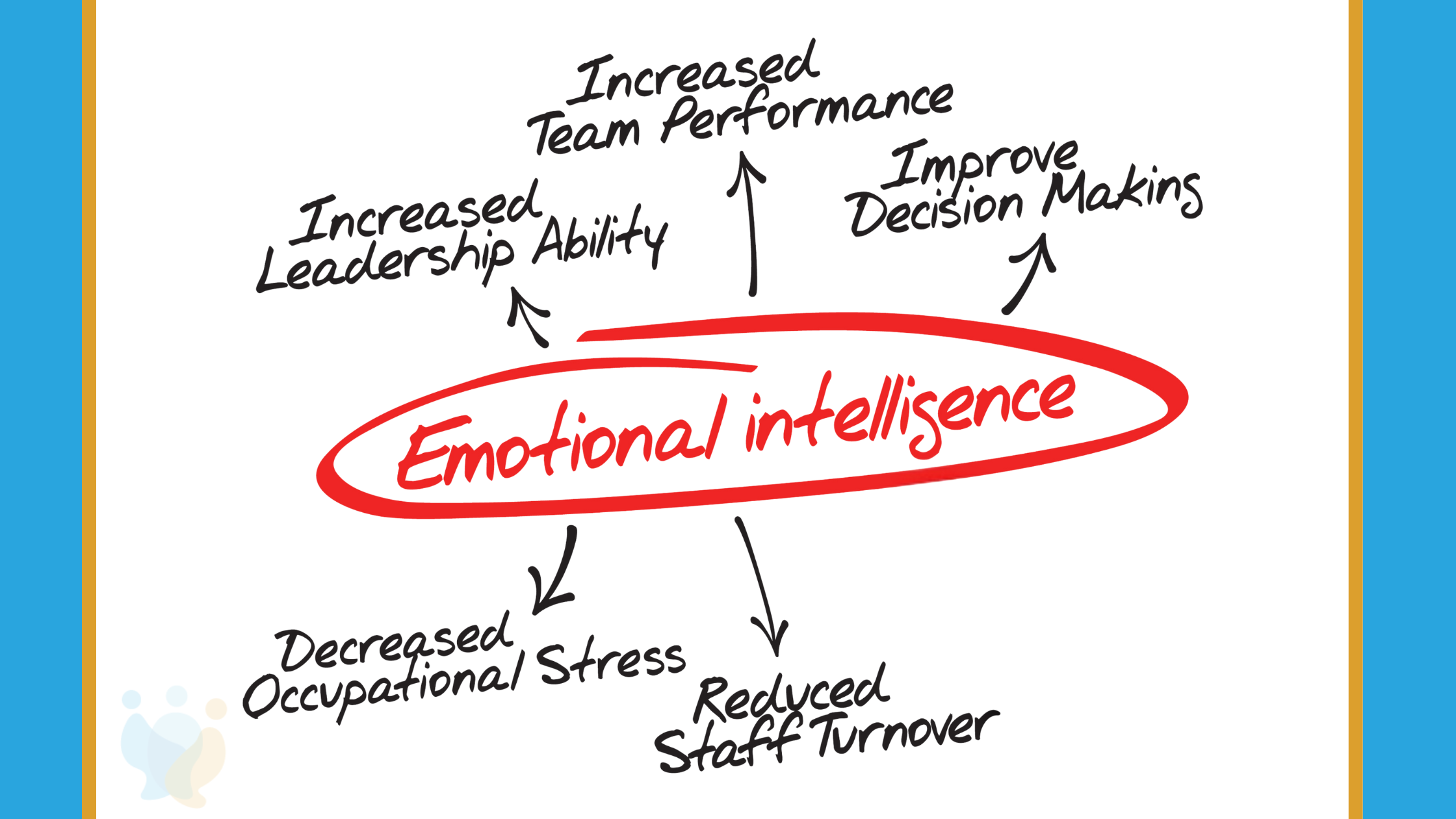
Skills for Sustaining Your Gift
- Professional support for your own mental health. Therapists need therapists. Counselors need counselors. This isn’t optional.
- Physical care as spiritual practice. Exercise reduces burnout risk by 85% in Kenyan studies. Your body is your instrument.
- Mindfulness and centering practices. Not New Age fluff,evidence-based tools to stay grounded.
- Boundary-setting without guilt. Saying no to preserve your yes. This is stewardship of your calling.
- Peer communities. You need people who understand the weight. Isolation kills.
- Trauma processing support. Compassion fatigue and vicarious trauma need specialized care.
What Strong Organizations Do
If you lead caregivers, here’s your responsibility:
- Build in clinical supervision and group debriefing
- Address staffing, reasonable caseloads matter
- Compensate fairly for emotional labor
- Create actual wellness programs, not token gestures
The evidence: In Migori County, organizations that implemented the CPIPE intervention reported significant reductions in burnout. Peer supervision programs show measurable improvement in caregiver wellbeing.
Sustainable caregiving is possible. But it requires training.
These practices take time to build. But you don’t have to wait to start. Here are three things you can do right now, today, to begin your restoration.
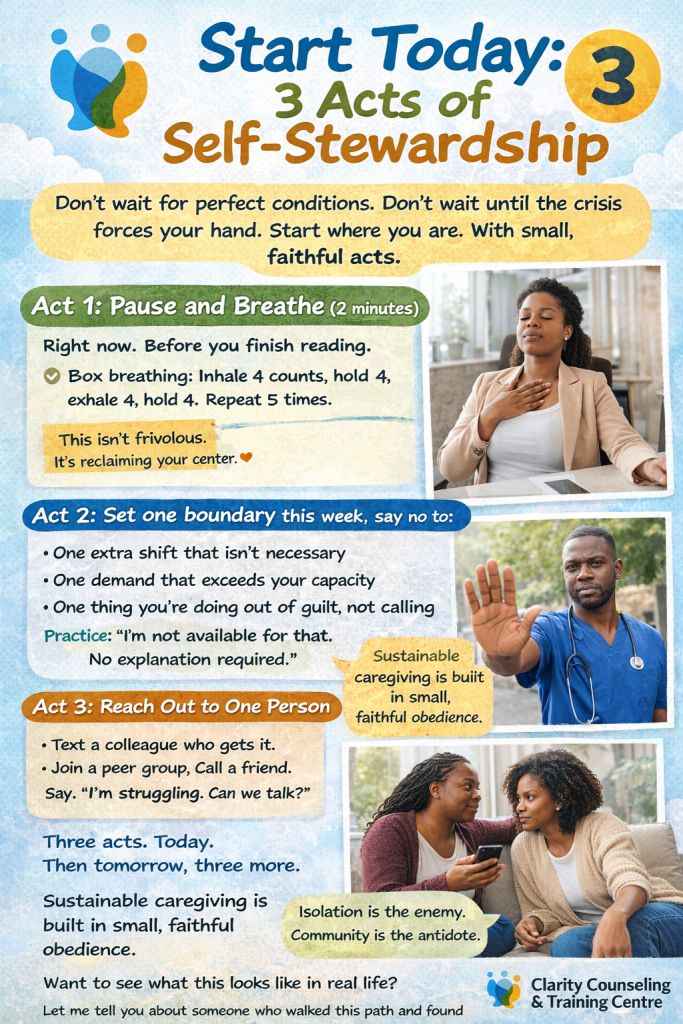
Start Today: 3 Acts of Self-Stewardship
Don’t wait for perfect conditions. Don’t wait until the crisis forces your hand.
Start where you are. With small, faithful acts.
Act 1: Pause and Breathe (2 minutes)
- Right now. Before you finish reading.
- Box breathing: Inhale 4 counts, hold 4, exhale 4, hold 4. Repeat 5 times.
This isn’t frivolous. It’s reclaiming your center.
Act 2: Set one boundary this week, say no to:
- One extra shift that isn’t necessary
- One demand that exceeds your capacity
- One thing you’re doing out of guilt, not calling
Practice: I’m not available for that. No explanation required.
Act 3: Reach Out to One Person
- Text a colleague who gets it. Join a peer group. Call a friend.
- Say: I’m struggling. Can we talk?
Isolation is the enemy. Community is the antidote.
Three acts. Today. Then tomorrow, three more.
Sustainable caregiving is built in small, faithful obedience.
Want to see what this looks like in real life? Let me tell you about someone who walked this path and found her way back.
Your Story: What Rebuilding Actually Looks Like
You didn’t quit caregiving.
You quit the version of caregiving that was killing you.
You called Clarity Counseling & Training Centre on a Tuesday afternoon.
The voice on the other end was warm. No judgment.
Just: When can you come in?
First session:
Soft lighting. A window overlooking trees. A tissue box within reach.
Your therapist, another counselor who’d been where you are, sat across from you.
No clipboard. Just presence.
You tried to explain. The words came out broken.
I’m supposed to help people. But I… I can’t…
Your therapist leaned forward.
You’ve been holding everyone else’s pain. Who’s been holding yours?
That question broke something open. You cried for forty minutes.
Three months later:
You still counsel. But everything’s different.
You joined a peer supervision group, six counselors who meet every other week to carry each other’s weight.
You learned the pause: 2 minutes between clients. Sit. Breathe. Release the last story before taking on the next.
Sounds simple, but it saved you.
You set boundaries. No more than 5 clients daily. Tuesdays off.
When you say no now, you don’t apologize.
You are sleeping through the night again.
Not every day is easy. But you are not drowning.
Now you tell every burnt-out caregiver you meet:
You don’t have to choose between caring for others and caring for yourself. You get to do both. But you have to learn how.
This could be your story too. And you don’t have to walk this path alone.
Let Us Help You Rebuild: Professional Support for Kenyan Caregivers
If you’re reading this and recognizing yourself.
You don’t have to figure this out alone.
You became a caregiver because you have a gift. Our job is to help you sustain it.
Clarity Counseling & Training Centre
Equipping Kenya’s Caregivers for Sustainable Service
We’re a NITA-accredited and KCPA-accredited counseling and Training Centre based in Nairobi.
We’ve walked alongside 1,200+ caregivers and trained 350+ professionals.
We partner with Jesuit Refugee Service, HESED Africa, SDI Kenya, and healthcare facilities across Kenya.
We Offer:
- Individual therapy for burnout, compassion fatigue, and vicarious trauma
- Group therapy and peer supervision for caregivers
- Debriefing sessions for processing traumatic experiences
- Professional training in sustainable caregiving practices
- Organizational wellness programs for healthcare facilities and NGOs
Your first consultation is FREE (15 minutes). Start this week.
Early intervention is 3x more effective than waiting for a crisis.
Join the 350+ caregivers who’ve learned to serve without self-destruction.
Online and in-person sessions available across Kenya.
You were called to this work. Let us help you sustain the calling.
| START YOUR RESTORATION TODAY
📍 Location: Finance House, Loita Street, Nairobi 🌐 Website: www.claritycounseling.co.ke 📧 Email: [email protected] 📞 Phone: +254 114444300 💬 WhatsApp: 0101515101 Available for booking FREE 15-minute consultation. No pressure. Just support. Book online or call today. |
The alarm will go off again tomorrow.
But tomorrow doesn’t have to look like today.
Additional Support Resources in Kenya
- Kenya Psychological Association: Professional referrals
- Befrienders Kenya: +254 722 178 177 (24/7 crisis support)
- Mental Health Kenya: www.mentalhealthkenya.org
- Africa Mental Health Foundation: Support groups and resources